Andrology and male fertility services
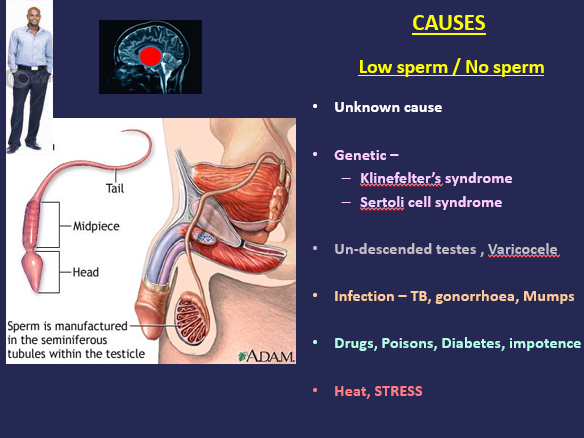
Infertility is defined as failure to achieve pregnancy after one year of unprotected intercourse. About 15% of couples are considered infertile, up to 40% of these are due to female factors alone, 30% due to male factors alone, 10% due to a combination of female and male factors, and 20% unexplained. Male factors are still generally poorly under-diagnosed and undertreated. About 90% of male associated infertility is untreatable and efforts to improve sperm count are largely anecdotal, except in cases of confirmed non-genetic vas deferens obstructions, reversal of vasectomy, infections, and confirmed hypogonadotropic hypogonadism. If no natural conception majority will require interventions with assisted conception techniques to achieve pregnancy. Recent experience in stem cell physiology suggests future in vitro generation of sperm cells for egg human fertilisation. Causes of male infertility Causes generally can be divided into pretesticular, testicular, and posttesticular.
- Pretesticular causes: Congenital or acquired diseases hypothalamus (hypogonadotropic hypogonadism), pituitary (abnormal sex hormones secretions), or peripheral organs (adrenals) that alter the hypothalamic-pituitary axis.
- Primary Testicular causes: Chromosomal or non-chromosomal with sex chromosomes or autosomal disorders.
- Posttesticular causes: include congenital blockage of the ductal system associated with cystic fibrosis (congenital bilateral absence of vas deferens, CBAVD), acquired blockage of the ductal system, antisperm antibodies, ejaculatory duct obstruction and retrograde ejaculation.
- Investigations.
- General examination– Look for a normal secondary sexual characteristics and signs of endocrine disorders.
- Chest examination looking for gynaecomastia
- Abdominal examination: for tumours, tenderness that can lead to testicular dysfunctions e.g, abdominal tuberculosis.
- Testicular examination – Prader orchidometer testicular volume normal considered to be greater than 20 mL or ultrasonography: for tumour masses or swellings, tenderness as a result infections, degenerative disease, cancer, atrophy etc.
- Testicular biopsy: for histology (usually needs referral for urologist care) to rule out benign infective, idiopathic or cancerous growths.
Treatments for options is based on the aetiology of the male Infertility
Replacement drug treatments: the use of androgens (mesterolone), FSH injections, clomiphene, steroids, and antioxidants (vitamins E and C). Mostly of these treatments may not be effective.
Other treatment modalities include
Intrauterine Insemination
Intracytoplasmic Insemination
Sperm retrieval usually for ICSI (TESA or PESA)
Donor-insemination
Adoption
Call the us today for male fertility health check up:
more information about our fertility & IVF, gynaecological and obstetrics services or to book an appointment with us.
What our patients say:
I’ve never been so low, when I was diagnosed with low sperm count. Thanks for the successful treatments. You restored my confidence.
Comparing IVF treatment prices here and elsewhere, I picked Fertility Assyst. My wife and l have John our son now! Thanks for your support and counselling all the way!
Thanks Dr Akinola and team. Your intervention was excellent and positive. We never felt disappointed at any stage. We look forward to start our ICSI treatment very soon.